Stages of Labour Guide: From Early Labour to Delivery
In the journey of childbirth, understanding the three stages of labour (and the four phases) helps prepare you for the big day. From the anticipation of early contractions to the transition phase of labour, each stage marks a significant milestone towards the ultimate moment of delivery. In this article, we’ll give you information on each of the stages of labour, the average labour time, and some tips to help you manage each stage. Join us as we navigate through the miraculous process of bringing new life into the world.
How Many Stages of Labour Are There?
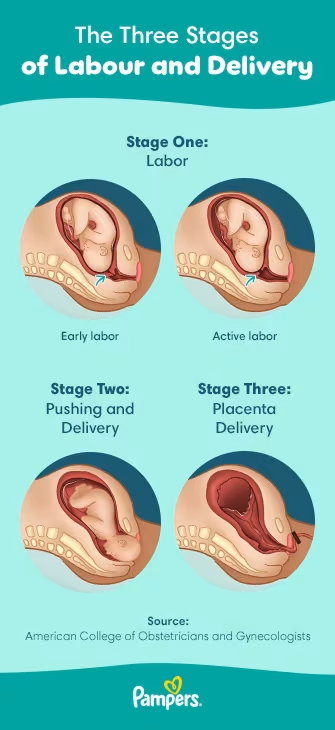
Childbirth, which consists of labour and delivery, is divided up into several stages, which can also be split into phases. Many parents-to-be wonder how many stages of labour there are; are there 3 or 4? This can be tricky to keep straight, but there are 3 labour stages, with the first stage divided into two phases. So, technically, there are 4 phases of labour:
Stage One: Labour
Early labour
Active labour
Stage Two: Pushing and delivering the baby
Stage Three: Placenta delivery
Below we’ll go into depth regarding each stage of childbirth labour and delivery so you get a better idea of what to anticipate. Just remember that every birth is unique, so what is considered a typical labour and delivery might not be exactly what you’ll experience. You may also want to check out some tips and advice to help prepare for labour and delivery.
What Is the First Stage of Labour (Stage 1)?
The first stage of labour has two phases: early labour and active labour. So, when does labour start? It’s difficult to pinpoint the exact start of labour, but it’s typically when you’re timing contractions and find that they are occurring every 5 to 15 minutes, lasting around 60 to 90 seconds. As for early labour vs. active labour, the transition between these phases usually happens once you’re dilated to 6 centimetres. Though there’s no stage called “prelabour,” you can consider early signs of labour, such as having contractions that are shorter and set further apart, to be the time before labour officially begins.
Birthing Classes This 9-part series, led by clinical childbirth experts, provides in-depth information for new parents on all stages of childbirth. Learn more
What Is Early Labour?
Early labour is when your contractions start to occur at regular intervals and your cervix experiences dilation and effacement. It’s the start of the birth process, and you’re probably not at the hospital yet. In early labour, your contractions
are about 5 to 15 minutes apart
last 60 to 90 seconds.
As early labour progresses, those contractions will get closer and closer together. You might not know what contractions feel like if you’ve never experienced them before, so you may not know what to anticipate. Unlike Braxton Hicks, which are false contractions, true contractions feel like pain or pressure and occur like this:
Pain or pressure starts in your lower back, moving around and toward your lower belly.
Your belly might feel tight and hard.
In between contractions, you will likely feel the same area relax and soften.
How Long Does Early Labour Last?
The first stage of labour tends to last the longest. No two pregnancies are the same, so it’s helpful to consider the entire first stage of labour as one interval. If this is your first delivery, the average labour time for this phase is 6 to 12 hours. It can be longer, of course, lasting up to 20 hours for first-timers. If you’ve given birth before, labour tends to be a little shorter but could still last up to 14 hours.
Early Labour: What Can You Do?
As far as stages of birth go, this initial phase of labour is an exciting time. It’s when everything starts to feel real! So, what can you do to support yourself during early labour? Here are a few ideas:
Take a stroll.
Relax with a bath or shower.
Play music that helps you calm down.
Practice any relaxation techniques or breathing methods you’ve learned.
Move often, changing your position.
Tips for Labour Partners If you’re a labour partner (the father of the baby, the baby’s grandma, the life partner of the person giving birth, etc.), you are an important part of the process! If possible, keep your pregnant partner distracted with activities like playing cards or a game. Give them a gentle shoulder massage or prepare a warm or cold compress they can apply to their lower back. You can also help with timing contractions. |
What Is Active Labour?
After this first stage of labour comes the transition to active labour. So, when does active labour start? Though everyone is different, the signs of active labour are when your
contractions are stronger
contractions are closer together
cervix is dilated at 6 centimetres.
When these three conditions occur, it could be time to head to the hospital or birth centre. That’s because during active labour, things can move quickly, and your cervix dilates rapidly during this labour stage.
Before you check in, the staff will determine whether you're in true active labour by taking steps such as tracking the timing of your contractions or performing a pelvic exam. Your medical team will also be checking your vital signs, your baby’s position, and your little one’s heart rate.
Though one of the most important active labour signs is dilation of 6 centimetres, it’s during this labour stage that your cervix will continue to dilate to 10 centimetres. Active labour can last as little as four hours or as long as eight hours or more. Other signs of active labour include:
Your water breaking (if it hasn’t already)
Stronger contractions that are two to three minutes apart and lasting anywhere from 30 to 70 seconds
Back pain
Leg cramps
Feeling nauseated
An urge to push (but it’s not time for that yet!).
Active Labour: What Can You Do?
The process of giving birth, especially during active labour, can be a waiting game. You’re waiting for your cervix to be 10 centimetres dilated before you can move on to the second stage of labour, which is pushing and delivery. So, what can you do during these active labour hours? After checking with your healthcare provider and getting the OK, you could do the following:
Practice relaxation techniques and breathing exercises you may have learned in your childbirth classes
Walk the halls of the hospital or birth centre
Take a shower or sit in a water bath
Pee often to empty your bladder
Resist the urge to push (pushing too soon can cause swelling, pain, and tearing)
Sip clear liquids, such as water, fruit juice without pulp, tea, etc., but avoid eating any solid food.
Tips for Labour Partners During the active labour phase, you as the labour partner can help facilitate those relaxation and breathing exercises. Other ways to help include applying firm pressure onto your partner’s lower back and massaging it, flexing their feet to help relieve cramping, and acting as the focal point during contractions. |
What Is the Second Stage of Labour (Stage 2)?
During which stage of labour is the fetus delivered, many parents-to-be wonder. That would be stage 2—surely the most exciting phase of giving birth! This birth stage includes pushing and delivery and begins when you’re 10 centimetres dilated and labour pains intensify. As every labour experience is different, it's a good idea to discuss pain management with your healthcare provider beforehand, such as when you're preparing your birth plan.
If you’re having a vaginal birth, you'll know it’s time to start pushing when
Your healthcare provider confirms that you’re fully dilated
Your body feels the urge to start truly pushing
Your contractions feel a little different, stronger and more painful, coming about every two to five minutes and lasting 60 to 90 seconds.
Though the average time of this stage of labour is often shorter than the first stage, lasting anywhere from mere minutes to two or three hours, it’s intense. If you’re a first-time parent pushing for more than three hours, or if you’ve given birth before and pushing for more than two hours, your healthcare provider may suggest
an assisted vaginal delivery (using forceps or a vacuum device)
turning your baby into a better birthing position (if, say, the baby is in a breech position)
How long after getting an epidural does the baby come? If you opt for an epidural, this stage may be allowed to go on longer without the interventions listed above, as long as your body is making progress.
Second Stage of Labour: What Can You Do?
Unlike the first labour stage, this phase is all about pushing, so you’ll be with your healthcare provider and medical team (and labour partner if you opt to have one), settled in your desired delivery position while listening to their instructions. Here’s how stage 2 of the birth process typically goes:
When contractions occur, you'll be instructed to bear down on them while pushing.
As your baby’s head appears, you might feel stinging or burning as the opening of your vagina (perineum) stretches, which is totally normal.
Once your little one’s head is completely out of the birth canal, you’ll continue pushing as instructed to deliver each shoulder.
After the shoulders are out, things tend to go fast, and your sweet new baby will be delivered fairly quickly at this point.
Your healthcare provider will check your baby, and then they or your labour partner will cut the umbilical cord.
Tips for Labour Partners Stage 2 is often the hardest stage for your partner, so being there for them is important. Supporting their body (depending on the birth position) will help them along the way, as will simply holding their hand and offering encouraging words. Discuss what kind of support they’d like ahead of time, so you know what to do, and know that they might change their mind! |
What Is the Third Stage of Labour (Stage 3)?
Stage 3 (or phase 4), the last stage of labour and delivery, occurs when your baby is fully delivered, and it’s time to push out the placenta. In terms of what to expect after giving birth, this labour stage, which is the shortest stage, could last up to about 30 minutes or so. You’ll still feel contractions but they’ll be far less painful and much closer together. Their purpose is to help the placenta detach from your uterus.
Once separated from the uterus wall, the placenta moves down into the birth canal and eventually to the vagina. Once again your healthcare provider will instruct you to bear down and push. The provider may even assist you by gently guiding the placenta out.
Once the placenta is out, you still might feel some contractions in your uterus. The body is truly amazing, as these contractions help the uterus slowly shrink and naturally seal the blood vessels. Your healthcare provider might give you some medication or massage your stomach to help with this process so as not to lose too much blood.
Tips for Labour Partners This is the fastest and likely less painful stage of labour, but it’s still a stage. Perhaps you’ll want to hold and admire the new baby, but don’t forget about your partner! Holding the baby is definitely a way to help, but if the little one is off getting tests, you can support your partner through their final contractions and pushes. You can wipe their brow, massage their shoulders, and offer encouraging words. |
How Long Does Labour Last?
How long does it take to push a baby out? What’s the average delivery time for a first baby? Again, every pregnancy and labour experience is different, so the duration of the 3 stages of labour and the total amount of time involved will vary from person to person.
However, there are some general timing ranges to keep in mind to help you prepare and know what to anticipate.
First stage of labour. The average labour time for the early labour phase of the first stage for first-timers can last anywhere from 6 to 12 hours, though for some, it can take up to 20 hours, so it’s quite a range. If you’ve given birth before, the process usually goes faster but can still last up to 14 hours. The second phase, active labour, can last from four to eight hours whether you’ve given birth before or not.
Second stage of labour. Once you start pushing, it's possible that you can meet your new baby in a matter of minutes! But the pushing and delivery phase of labour can also last a longer time, up to two or three hours.
Third stage of labour. This labour stage can be quick, lasting up to 30 minutes.
The American College of Obstetricians and Gynecologists offers the following estimations:
First delivery: 12 to 18 hours on average
Second+ delivery: 8 to 10 hours on average
Remember, no matter how long it takes, in the end you’ll still meet your little one!
Stages of Labour and Delivery Timeline Chart
Here’s a timeline and easy-to-read chart to help explain the 3 stages of labour. You can also download a copy to have the information readily available for when you need it.
Stages of Labour Timeline Chart
| Stage | First Stage | Second Stage | Third Stage |
|---|---|---|---|
| What is it? | Early labour, active labour | Pushing and delivery | Delivering the placenta |
| When does it start? | Early labour: when contractions are every 5 to 15 minutes, lasting around 60 to 90 seconds. Active labour: contractions become longer and closer together, and when you are 6 centimetres dilated." | Stronger, more intense contractions and when you’re 10 centimetres dilated. | After your baby is delivered and your placenta has reached your vaginal opening. |
| How long (first delivery) | Early labour: 6 to 12 hours (or 20+ hours) Active labour: 4 to 8 hours | Up to 2 or 3 hours | Up to 30 minutes |
| How long (second+ delivery) | Early labour: varies but is usually less than the first delivery Active labour: 4 to 8 hours | Up to 2 or 3 hours | Up to 30 minutes |
| What happens? | Early labour: count contractions and manage pain. Active labour: head to the hospital or birth centre and wait for your cervix to dilate from 6 to 10 centimetres." | You’ll bear down and push during your contractions, as instructed by your healthcare provider. | You’ll experience light contractions to detach the placenta, then push when instructed to deliver the placenta. |
| What you can do | Breathing and relaxation exercises, walking, showering or bathing, listening to music, changing positions often, and sipping clear liquids but peeing often. | Breathing, epidural block or other pain medication (if desired), concentrating on your labour partner or healthcare provider. | Breathing and relaxation exercises. |
| How a labour partner may help | Massages, counting and helping with contractions, distracting with games or conversation, and applying cold and warm compresses. | Support the birthing position, hold a hand, help with contractions, and offer encouraging, supportive words. | Helping with any lingering contractions, massaging your partner’s shoulder, wiping their brow, and offering supportive words. |
FAQS AT A GLANCE
The three stages of labour are as follows:
- First stage of labour: early labour and active labour
- Second stage of labour: pushing and delivery
- Third stage of labour: delivering the placenta.
The Bottom Line
As you get ready for delivery, it helps to know a little more about each of the 3 stages of labour (or the 4 phases of labour). Though everyone is different, you can at least get a better idea of what each stage entails, what you can do during the stage, what to expect from your healthcare provider, and what your labour partner can do to help. We hope this article gives you some peace of mind, knowing your little one will eventually be on their way! In the meantime, enjoy those final moments of pregnancy. As you prepare for your baby’s arrival, don’t forget to sign up for the Pampers Club app, where you can get discounts on what every parent needs: diapers and wipes.
How We Wrote This Article The information in this article is based on expert advice found in trusted medical and government sources, such as the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists. You can find a full list of sources used for this article below. The content on this page should not replace professional medical advice. Always consult medical professionals for full diagnosis and treatment.
Join Pampers Club and get:




 PAMPERS COUPONS
PAMPERS COUPONS TOOLS & QUIZZES
TOOLS & QUIZZES PARENTING TIPS
PARENTING TIPS